Fecha de recepción: 5 de octubre de 2023 Fecha de aceptación: 30 de noviembre de 2023
REVISIóN
https://dx.doi.org/10.14482/sun.40.02.411.999
Neurological Manifestations of Systemic Diseases: Key Aspects for the Clinician
Manifestaciones neurológicas de enfermedades sistémicas: aspectos claves para el clínico
Daniel S. Marín-Medina1, Alejandro Almeida-Guerrero2 , Jorge Iván Castaño Gutiérrez3, Adriana Paola Ortega-Quintero4
1. Daniel Stiven Marín-Medina. MD, Universidad Tecnológica de Pereira. Pereira. 4th year neurology resident, Universidad Nacional de Colombia, Bogotá. Affiliation: NeuroUnal Research Group, Universidad Nacional de Colombia, Bogotá, Bogotá D.C., Colombia. E-mail: dmarinme@unal.edu.co. ORCID: https:// orcid.org/0000-0002-9077-6309. CVLAC: https://scienti.minciencias.gov.co/ cvlac/visualizador/generarCurriculoCv.do?cod_rh=0001508113
2. Alejandro Almeida Guerrero. MD, Universidad Tecnológica de Pereira. Pereira. -2nd year internal medicina resident, Universidad de Caldas Manizales, Colombia Affiliation: Facultad de Ciencias de la Salud. Universidad Tecnológica de Pereira. Pereira, Risaralda, Colombia. E-mail: alejandroalmeida33849@ucaldas. edu.co. ORCID: https://orcid.org/0000-0001-7824-481X. CVLAC: https://scienti.minciencias.gov.co/cvlac/visualizador/generarCurriculoCv.do?cod_rh=0000183240
3. Jorge Iván Castaño Gutiérrez. MD, Universidad Tecnológica de Pereira. Pereira. Affiliation: Facultad de Ciencias de la Salud. Universidad Tecnológica de Pereira. Pereira, Risaralda, Colombia. MSc in Epidemiology. jorgecastg@gmail.com. ORCID: https://orcid.org/0000-0001-7837-6305. CVLAC: https://scienti.minciencias.gov.co/cvlac/visualizador/generarCurriculoCv.do?cod_rh=0001735360
4. Adriana Paola Ortega Quintero. MD, Universidad Industrial de Santander, Bucaramanga Colombia. Internist, Universidad Nacional de Colombia, Bogotá Colombia. Affiliation: Departament of Internal Medicine, Clínica Keralty Ibagué, Ibagué Colombia. aortegaq@unal.edu.co. ORCID: https:// orcid.org/0009-0007-1042-6653. CVLAC: https://scienti.minciencias.gov.co/cvlac/visualizador/ generarCurriculoCv.do?cod_rh=0002163837
Corresponding author: Daniel Stiven Marín-Medina. NeuroUnal Research Group, Universidad Nacional de Colombia, Bogotá, Bogotá D.C., Colombia. E-mail: dmarinme@unal.edu.co
ABSTRACT:
The nervous system interacts with all other systems in the human body on a continuous basis. It's not uncommon for a disease to exhibit neurological symptoms that are not solely attributable to a primary nervous system disorder, but, rather, to the intricate relationships the nervous system has with other organs. This article reviews how diverse gastrointestinal, endocrine, rheumatic, kidney, heart, and other affections manifest in the neurological system. Key points, frequent symptoms, and signs are thus summarized to provide a comprehensive understanding of the relationship between systemic diseases and neurological symptoms. Emphasizing the clinical presentation of a selected group of conditions, it is hoped that clinicians can better recognize the potential for neurological symptoms in patients with systemic diseases, and the potential for systemic diseases in patients exhibiting neurological symptoms, leading to earlier diagnosis and improved outcomes.
Keywords: endocrine system diseases; gastrointestinal diseases; heart diseases; kidney diseases; neurology; neurologic manifestations; rheumatic diseases.
RESUMEN:
El sistema nervioso interactúa de forma continua con todos los demás sistemas del cuerpo humano. No es raro que una enfermedad muestre síntomas neurológicos que no son atribuibles únicamente a un trastorno primario del sistema nervioso, sino más bien a las intrincadas relaciones que tiene el sistema nervioso con otros órganos. Este artículo revisa cómo diversas afecciones gastrointestinales, endocrinas, reumáticas, renales, cardíacas, entre otras, se manifiestan en el sistema neurológico. Los puntos clave, los signos y síntomas frecuentes se resumen aquí para brindar una comprensión integral de la relación entre las enfermedades sistémicas y los síntomas neurológicos. Al resaltar las manifestaciones clínicas de un grupo seleccionado de enfermedades, se espera que los médicos puedan reconocer mejor el potencial de síntomas neurológicos en pacientes con enfermedades sistémicas y, por el contrario, el potencial de enfermedades sistémicas en pacientes que presentan síntomas neurológicos, lo que llevaría a un diagnóstico más temprano y mejores resultados.
Palabras clave: diagnóstico; enfermedad; manifestaciones neurológicas; medicina interna; neurología.
INTRODUCTION
The nervous system plays an integral role in the human body, and its interactions with other systems are crucial for maintaining overall health. When the nervous system is compromised, it can lead to a myriad of symptoms that can be difficult to diagnose. Although neurological symptoms are often associated with primary nervous system disorders, they can also be caused by systemic diseases that affect other organs in the body. As such, it is essential to understand the complex relationships that exist between the nervous system and other organ systems to provide an earlier diagnosis and effective treatment for patients exhibiting neurological symptoms. This review focuses on how diverse cardiac, gastrointestinal, endocrine, and other conditions manifest in the neurological system. Figure 1 summarizes key neurological manifestations related to the systemic diseases mentioned in this paper.
The review was conducted by researching academic articles published in the past 20 years in leading online databases such as MEDLINE, Embase, Scopus, Science Direct, Scielo, and Google Scholar. It included different types of studies published in English and Spanish, including systematic reviews, meta-analyses, review articles, case reports, and observational studies, as well as articles identified through bibliographic references. The search utilized terms such as neurologic or neurological manifestation and systemic diseases, renal disease, cardiac disease, hepatic disease, rheumatology disease, endocrine disease, and gastrointestinal disease.
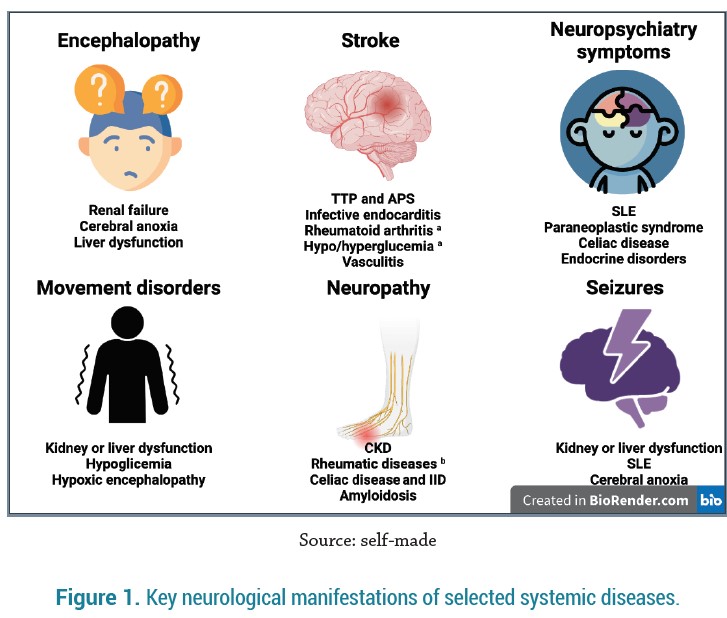
a Stroke-like (acute focal deficits)
b Mainly Sjögren syndrome, ANCA vasculitis, SLE and RA.
APS: antiphospholipid syndrome; CKD: chronic kidney disease; IID: inflammatory intestinal disease; RA: rheumatoid arthritis; SLE: systemic lupus erythematosus; TTP: thrombotic thrombocytopenic purpura.
KIDNEY DISEASES
1. Renal Failure
Neurological involvement in chronic kidney disease (CKD) has a slow progression, while in acute kidney failure and acute decompensation of CKD, changes are more accentuated [1].
Initial symptoms are nonspecific and fluctuating; these include fatigue, apathy, irritability, headache, and altered states of consciousness that change throughout the day. Afterwards, emotional lability, personality changes, sleep disorders, and memory impairment appear.
Advanced stages manifest with delirium, hallucinations, stupor, and coma [1]. Always bear in mind the possibility of renal encephalopathy in a patient with kidney disease who develops fluctuating consciousness or cognitive impairment.
Cognitive deficits can occur in up to 80% of the patients with CKD, and they manifest with memory and executive function disorders, such as problem-solving or calculating difficulties [2]. Movement disorders can also be seen and include tremor, restless legs syndrome, asterixis, para-tonia (semi-voluntary increase in muscle tone), and multifocal myoclonus [3]. A third of the patients can present with focal, generalized, and non-convulsive epileptic seizures, particularly in patients that develop posterior reversible encephalopathy syndrome (PRES) [4]. Sixty percent of the patients develop polyneuropathy with pruritus, dysesthesias, impaired vibration, and temperature sense, hyporeflexia, distal weakness, and autonomic symptoms [5].
Dialysis disequilibrium syndrome is a complication that occurs in patients undergoing renal replacement therapy, typically presenting at the end of dialysis, and resolving within a few hours. It is more common in first-time dialysis patients, or in those who skip sessions [1].
2. Microangiopathy
Around 60% of patients with thrombotic thrombocytopenic purpura experience initial neurological symptoms such as headache, confusion, focal deficits, seizures, and coma [6]. Hemolytic uremic syndrome is characterized more by renal compromise rather than neurological symptoms (25%-30%), with patients presenting with lethargy, irritability, seizures, and, less frequently, focal deficits, cortical blindness, and coma [7]. PRES can be present in both diseases and should be considered when a patient with kidney failure develops acute neurological symptoms and has fluctuating blood pressure, a history of cytotoxic drug use, autoimmune alterations, or pre-eclampsia-eclampsia [4].
RHEUMATIC DISEASES
1. Systemic Lupus Erythematosus (SLE)
Neuropsychiatric manifestations can occur in 28-40% of patients, either before or at the time of diagnosis, and it usually manifest as a first psychotic episode in patients without a psychiatric history [8]. Other central nervous system (CNS) symptoms could be attributed to SLE, complications derived from therapy, or coexisting pathologies such as antiphospholipid syndrome. These symptoms include headache (37%), mood disorders (15%), cognitive dysfunction (23-60%), seizures (8%), and cerebrovascular diseases (CVD) (7%). Involvement of the peripheral nervous system (PNS) is less frequent, and it can manifest as symmetric or asymmetric distal sensorimotor neuropathy, cranial neuropathy, or mononeuritis multiplex [12].
2. Rheumatoid Arthritis (RA)
In advanced stages of RA, involvement of the cervical spine is common. This can lead to atlanto-axial or subaxial subluxation resulting from the inflammatory process. While it is usually asymptomatic, it may present with occipital pain, stiffness, and loss of cervical lordosis [10]. Vertical subluxation can lead to low cranial nerve involvement, paresthesia, and pyramidal syndrome [10]. Although infrequent, CNS involvement can also manifest as psychiatric disorders, cognitive dysfunction, depression, anxiety, headache, an increased risk of epilepsy, and, in rare cases, aseptic meningitis, or stroke-like episodes [9]. Neuropathy is common, occurs in 20% of patients, and can present as entrapment (such as carpal tunnel syndrome), mononeuritis multiplex, or senso-rimotor distal neuropathy [9,10].
3. Sjögren Syndrome (SS)
Neurological involvement occurs in 20% of cases with SS, and it typically appears before the onset of xerostomia and xerophthalmia [9, 11]. PNS involvement is quite common and should always be suspected in patients with SS and sensory symptoms. Symmetric-sensitive polyneuropathy manifests with paresthesia in the lower limbs, loss of sensitivity, and hyporeflexia [11]. Other forms of PNS involvement include sensorimotor polyneuropathy, multiple mononeuropathy, sensory ganglionopathy, small fiber neuropathy, cranial neuropathy, myositis, and autonomic alterations. CNS involvement is less frequent and includes cognitive alterations, meningitis, symptoms like multiple sclerosis, optic neuritis, and transverse myelitis [9,11].
4. Systemic Sclerosis and Scleroderma
In localized scleroderma, there is often significant muscular involvement (90%), and nearly half of patients with coup de sabre present epileptic seizures with altered consciousness that may progress to bilateral tonic-clonic seizures [12]. Neurological manifestations of systemic sclerosis include epileptic seizures, depression, anxiety, headaches, cognitive decline, peripheral sensorim-otor neuropathy, carpal tunnel syndrome. Systemic sclerosis should be suspected in patients with bilateral trigeminal neuropathy [12].
5. Mixed Connective Tissue Disease
The CNS involvement in mixed connective tissue disease is like that of SLE. Around 10-17% of patients may present with neuropsychiatric manifestations such as psychosis. Other neurological manifestations are trigeminal neuropathy, headaches, aseptic meningitis, epileptic seizures, peripheral neuritis, and cerebrovascular disease [13].
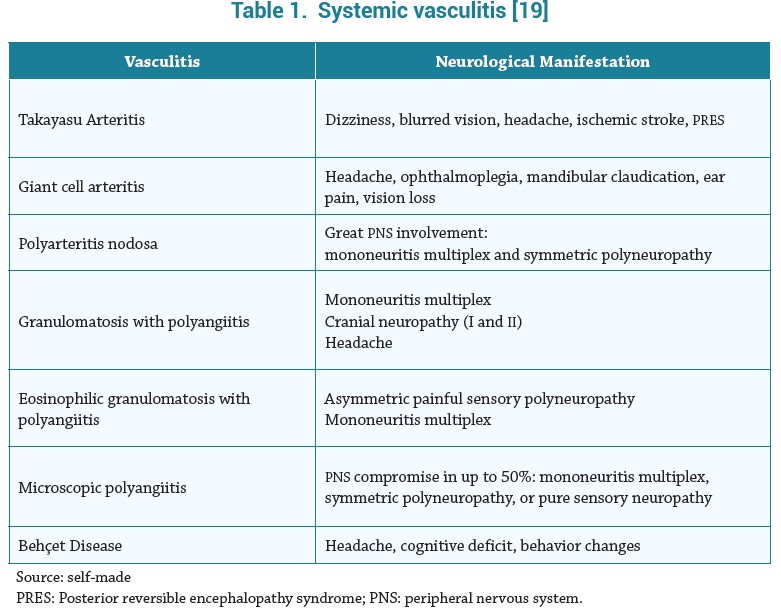
6. Vasculitis
The neurological manifestations of systemic vasculitis are summarized in Table 1. Non-systemic vasculitic neuropathy (organ-specific vasculitis) is not a rare form of vasculitis and most often presents as multiple mononeuritis, distal symmetric polyneuropathy, or pure sensory neuropathy [14]. Vasculitis should be suspected in any patient with multiple mononeuritis or polyneu-ropathy that begins insidiously and with progressive involvement of different territories [15].
7. ANTIPHOSPHOLIPID SYNDROME (APS)
Headache is the most common manifestation, with migraine being the most prevalent type (20%). CVD is the most severe and frequent complication, particularly in young patients. In some cases, venous sinus thrombosis can cause headache, nausea, focal deficit, seizures, and intracra-nial hypertension, as well as reversible cerebral vasoconstriction syndrome (RVCS) with thunderclap headaches [16]. APS should be suspected in young patients with CNS arterial or venous thrombosis without risk factors or genetic causes. Ocular syndromes, such as amaurosis fugax, occur in 15-88% of cases. Other manifestations include cognitive deficits, seizures, syndromes like multiple sclerosis, and psychiatric syndromes [17]. PNS involvement is rare.
ENDOCRINE DISEASES
1. Pituitary/hypothalamic Disorders
Hypopituitarism typically presents with asthenia, apathy, and decreased cognitive function. Functional adenomas can cause Cushing's disease with myopathy, behavioral changes, or acromegaly with apathy, depression, and sleep apnea/hypersomnia [18].
Pituitary apoplexy commonly presents with thunder retro orbital headaches (80%) and visual symptoms such as decreased visual acuity, visual field defects, and ophthalmoplegia [19]. Other symptoms may include fever, nausea, vomiting, altered consciousness, and meningeal signs [20]. In diabetes insipidus, the development of hypernatremia can lead to encephalopathy [21]. Always suspect diabetes insipidus in a critically ill patient that develops excessive thirst.
2. Adrenal Disorder
Neurological manifestations of adrenal insufficiency are nonspecific and can include neuropsy-chiatric symptoms such as depression, apathy, or delirium. Some patients may also experience muscle pain and weakness, as well as symptoms of intracranial hypertension like headaches. In cases of adrenal crisis, patients may develop seizures, severe encephalopathy, and myopathy [22]. Adrenal hyperfunction, such as Cushing's syndrome, can lead to intracranial hypertension, en-cephalopathy, and mood disorders such as mania-depression, insomnia, anxiety, and psychosis, along with associated myopathy [23]. Pheochromocytoma can cause explosive headaches, anxiety, psychosis, cognitive decline, tremors, and seizures [24].
Patients with neuropsychiatric symptoms who are young are frequently misdiagnosed with primary psychiatric illnesses or conversion/somatization syndromes. It is important to consider endocrine disorders as a possible cause of atypical psychiatric symptoms, especially in patients without known risk factors or with unexplained systemic symptoms.
3. Hypothyroidism and Myxedema Coma
Neurological complications of hypothyroidism can develop gradually and may initially present as cognitive impairment, neuromuscular deficits, or headache, with fatigue, apathy, drowsiness, and lack of concentration being common [26]. Hypothyroidism should always be ruled out in elderly patients with a recent onset of cognitive decline.
In myxedema coma, myopathy can cause weakness, slow contraction, and relaxation (pseudo-myotonia), asthenia, and fatigue. Other symptoms may include hearing loss and hoarseness [25]. The most severe cases can result in hypothermia and altered consciousness, with delirium, stupor, or coma [26]. Additional symptoms can include cerebellar signs and seizures [27].
4. Hyperthyroidism and Thyroid Storm
Thyrotoxicosis may often present with symptoms of motor restlessness such as akathisia, postural tremor, as well as psychiatric symptoms including anxiety, insomnia, mania, and less frequently seizures [27]. In elderly patients, it may present in the opposite way, with lethargy, stupor, or coma, which is known as 'apathetic hyperthyroidism'. In Grave-Basedow disease, ophthalmoplegia may appear and the involvement of the optic nerve is usually late [28]. Some patients may manifest neuromuscular disorders such as myopathy, periodic paralysis, and neuropathy, which often manifest insidiously.
In thyroid storm, encephalopathy commonly presents as agitation, emotional lability, confusion, paranoia, psychosis, and eventually coma. Additionally, cases of patients with epileptic status and cardiovascular disease have been reported [29].
5. Hyperglycemia
One neurological complication of diabetic ketoacidosis are cerebral edemas. Headache is one of the first symptoms, followed by rapid deterioration including lethargy, seizures, pupillary changes, respiratory distress, and manifestations of intracranial hypertension such as papilledema, high blood pressure, and bradycardia [30]. In hyperosmolar crisis, three neurological conditions can be recognized: focal deficits with crisis in the form of continuous focal seizure (epilepsia partialis continua), hemicorea/hemiballismus syndrome, and stupor/coma without neurological focus [31]. Always assess serum or capillary glucose in patients with focal deficits (stroke-like) or acute-onset abnormal movements.
In diabetes, it is common to have both PNS and autonomic involvement. The most frequent form is distal symmetric polyneuropathy, while other manifestations include cardiac autonomic neuropathy, gastrointestinal dysmotility, and impotence. Focal neuropathies, such as isolated mononeuropathies, radiculopathy, or polyradiculopathy, are less common but may also occur. In the CNS, diabetes is associated with stroke and cognitive impairment. Due to the complexity of the underlying mechanisms and the extensive manifestations of diabetic neuropathy, a detailed review is beyond the scope of this article, and we recommend further reading for a more comprehensive understanding. [32].
6. Hypoglycemia
In hypoglycemia, initial neurologic symptoms can include dizziness, fatigue, visual disturbances, and cognitive changes such as irrational and erratic behavior. If left untreated, hypoglycemia can lead to seizures and coma. In rare cases, hypoglycemia can cause focal neurologic deficits that mimic symptoms of stroke, so the previous advice for measuring serum or capillary glucose stands [33].
CARDIAC AND PULMONARY DISEASE
1. Ischemic and Hypoxic Encephalopathy
In cases of global cerebral ischemia, the first symptom is typically a change in consciousness, which can progress to coma after more than 4 minutes of hypoxia. Subsequently, decorticate or decerebrate postures, myoclonus, and seizures may appear [34].
Cerebral anoxia can lead to different movement disorders, including action myoclonus (Lance-Adams syndrome), parkinsonism, chorea, dystonia, ataxia, and seizures. Late hypoxic enceph-alopathy may develop after apparent recovery from cerebral anoxia. Symptoms such as listless-ness, confusion, irritability, occasional agitation, or mania may appear over a period of one to four weeks and may persist in a minority of patients [34].
2. Pulmonary Encephalopathy
Unspecific signs, such as headache, attention deficits, drowsiness, and cognitive deficits, may appear in chronic obstructive pulmonary disease (COPD) and cases of alveolar hypoventilation. If left untreated, these signs can progress to psychomotor agitation, nocturnal delirium, and ultimately confusion and coma in states of sustained hypercapnia [35]. Additionally, in some cases, asterixis and myoclonus may occur [35].
Around two years after resuscitation, approximately half of the patients who develop acute respiratory distress syndrome (ARDS) may experience neurocognitive disorders, including emotional disorders, anxiety, apathy, depression, and exacerbation of painful phenomena [36].
3. Infective Endocarditis
Neurological complications occur in 15% to 47% of patients with endocarditis. Among these, strokes are the most frequent and can be the initial presentation in about 20% of cases [37]. While most of these strokes are ischemic, subarachnoid, or intracerebral hemorrhages can also occur due to septic endarteritis, hemorrhagic transformation from an ischemic infarction, or rupture of a fungal aneurysm [38].
In young patients with risk factors for bacteremia who develop acute neurological deficits, it is important to always keep a high suspicion of septic embolism. This is because septic embolism can result not only in strokes but also in the direct infection of the central nervous system, potentially leading to meningoencephalitis, cerebritis, or abscess formation. These conditions can be recognized by the appearance of meningeal signs and sensory/motor deficits [37].
4. Aortic Dissection
Neurological complications occur in 25% of patients with aortic dissection [39]. In a small percentage of patients, neurological manifestations may be the initial finding or may be preceded by chest pain and eventually lead to the diagnosis of an extensive arterial dissection. Ischemic stroke is the most common neurological complication associated with type A dissections, but other potential complications include Horner syndrome (when the dissection extends to the carotid artery), left recurrent laryngeal nerve palsy, and spinal cord ischemia [40].
GASTROINTESTINAL DISEASES
1. Hepatic Encephalopathy (HE)
HE is a neurological complication that can occur in patients with liver dysfunction, particularly in those with cirrhosis. The initial and mild stages form of the disease may go unnoticed due to subtle manifestations that include changes in mental state, attention, and behavior. There are mainly two forms of presentation: acute and chronic encephalopathy. Acute encephalopathy is characterized by acute recurrent confusion episodes, while the chronic form, also known as non-wilsonian hepatocerebral degeneration, is characterized by cognitive decline and motor disorders such as parkinsonism, chorea, dystonia, asterixis, and myelopathy [41].
In patients with cirrhosis, mild HE with minimal changes occurs in 20% to 80% of the cases, and the main symptoms include work-related memory impairment and executive function impairment [42]. Always consider HE in a patient with liver disease or risk factors who develops fluctuating consciousness or cognitive impairment.
2. Celiac Diseases and Gluten Sensibility
Neurological dysfunction can be present in up to 22% of the patients, even without clear gastrointestinal symptoms [43]. Many symptoms are related to vitamin deficiencies (B1, B12, B6, E, B2, and B3), including cognitive decline, behavior disorders, attention deficit, chronic headache, and seizures. 33% of patients can develop distal symmetric peripheral neuropathy [44].
Other manifestations include myelopathy, cerebellar ataxia, and restless legs syndrome [43].
3. Intestinal Inflammatory Disease
The incidence of neurological complications in Crohn's disease and ulcerative colitis patients ranges from 0.25% to 37%. The most common neurological complication is axonal peripheral neuropathy. Both Crohn's disease and ulcerative colitis can present with focal or diffuse myositis before the onset of gastrointestinal symptoms. Due to a secondary deficiency of vitamin B12, progressive myelitis can be observed. Furthermore, patients with these diseases are at a higher risk for autoimmune events such as multiple sclerosis and CNS vasculitis [45].
OTHER DISEASES:
1. Sarcoidosis
Around 10% patients have neurological manifestations, 15% without systemic manifestation. Half of these patients develop cranial neuropathy, with the facial, optic, and vestibulocochlear nerve being the most affected. It is not uncommon for patients to also present with aseptic meningitis, acute encephalopathy, and hypothalamic dysfunction. Other neurological manifestations of sarcoidosis include myelopathy, myopathy, peripheral neuropathies with mononeuritis multiplex and Guillain-Barré syndrome [46].
2. Amyloidosis
Neuropathy is the most common neurological manifestation of light chain amyloidosis, affecting both small and large nerve fibers. Patients typically report paresthesia and burning pain in the lower limbs, which progresses to impairment of vibration and proprioception [47]. Facial cranial neuropathies and plexopathies have also been reported, and 65% to 75% of patients experience autonomic dysfunction, including diarrhea, postural hypotension, gastroparesis, and erectile dysfunction [48]. Hereditary forms of amyloidosis could manifest as familial bilateral carpal tunnel syndrome in patients without risk factors or comorbidities.
3. IgG4-related Disease
There is usually involvement of the orbit, pachymeningitis, hypophysis, and peripheral nervous system. The orbital disease is characterized by progressive chronic lacrimal gland and periorbital edema, which can progress to palpebral ptosis and diplopia. Meningeal impairment causes symptoms of intracranial hypertension and cranial neuropathy. Hypophysis involvement is associated with decreased libido, hypogonadism, hypothyroidism, and hypoadrenalism [49].
4. Lymphoma
About one-third of patients have some involvement of the nervous system. When the tumor directly invades the nervous system, symptoms depend on the location of the tumor and may include focal deficits, seizures, meningitis, intracranial hypertension, and syndrome of inappropriate antidiuretic hormone secretion. Indirect nervous system complications include paraneo-plastic syndromes. Subacute encephalitis could cause personality changes, seizures, psychosis, behavioral alterations, and sleep disturbances, while cerebellar degeneration could lead to symptoms such as ataxia.
Hypercoagulability complications, such as arterial and venous thrombosis can present with focal deficits and headaches. When the PNS is involved, it typically manifests as cranial neuropathy or lumbar radiculopathy. It is always crucial to consider other potential complications in the CNS and PNS that may be associated with chemotherapy or radiation therapy [50].
CONCLUSIONS
The nervous system can be affected by various conditions, including gastrointestinal, endocrine, rheumatic, lung, kidney, and heart diseases, among others. As a result, neurological symptoms are commonly seen in clinical practice due to systemic diseases, and conversely, common systemic diseases can frequently cause neurological manifestations. Therefore, it is crucial to keep in mind that a wide range of potential diagnoses should be considered when approaching neurological symptoms and signs. This approach can lead to an earlier diagnosis and more effective treatment for patients experiencing neurological symptoms.
Conflict of interest: None to declare.
Financing: by the authors.
Contribución de los autores: Diseño del estudio DSMM /AAG/JCG/APOQ - Revisión bibliográfica DSMM/AAG/JCG/APOQ - Preparación del manuscrito DSMM/AAG/JCG/APOQ - Revisión de la versión final DSMM /AAG/JCG/APOQ
REFERENCES
[1] Hocker SE. Renal Disease and Neurology. Continuum (Minneap Minn) 2017;23:722-43. doi: 10.1212/CON.0000000000000469.
[2] Barrett KM. Neurologic manifestations of acute and chronic renal disease. Continuum (Minneap Minn) 2011;17:45-55. doi: 10.1212/01.CON.0000394673.82619.24.
[3] Lacerda G, Krummel T, Hirsch E. Neurologic presentations of renal diseases. Neurol Clin 2010;28:45-59. doi: 10.1016/J.NCL.2009.09.003.
[4] Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol 2015;14:914-25. doi: 10.1016/S1474-4422(15)00111-8.
[5] Krishnan A V., Kiernan MC. Uremic neuropathy: clinical features and new pathophysiological insights. Muscle Nerve 2007;35:273-90. doi: 10.1002/MUS.20713.
[6] Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood 2017;129:2836-46. doi: 10.1182/BLOOD-2016-10-709857.
[7] Canpolat N. Hemolytic uremic syndrome. Turk Pediatri Ars 2015;50:73-82. doi: 10.5152/TPA.2015.2297.
[8] Muscal E, Brey RL. Neurologic manifestations of systemic lupus erythematosus in children and adults. Neurol Clin 2010;28:61-73. doi: 10.1016/J.NCL.2009.09.004.
[9] Dimberg EL. Rheumatology and Neurology. Continuum (Minneap Minn) 2017;23:691-721. doi: 10.1212/CON.0000000000000474.
[10] DeQuattro K, Imboden JB. Neurologic Manifestations of Rheumatoid Arthritis. Rheum Dis Clin North Am 2017;43:561-71. doi: 10.1016/J.RDC.2017.06.005.
[11] Perzyñska-Mazan J, Masliñska M, Gasik R. Neurological manifestations of primary Sjogren's syndrome. Reumatologia 2018;56:99-105. doi: 10.5114/REUM.2018.75521.
[12] Amaral TN, Peres FA, Lapa AT, Marques-Neto JF, Appenzeller S. Neurologic involvement in scleroderma: a systematic review. Semin Arthritis Rheum 2013;43:335-47. doi: 10.1016/J.SEMARTHRIT.2013.05.002.
[13] Hao Y, Feng L, Teng Y, Cheng Y, Feng J. Management of multiple neurological complications in mixed connective tissue disease: A case report. Medicine 2018;97. doi: 10.1097/MD.0000000000011360.
[14] Collins MP, Hadden RD. The nonsystemic vasculitic neuropathies. Nat Rev Neurol 2017;13:302-16. doi: 10.1038/NRNEUROL.2017.42.
[15]. Fukami Y, Koike H, Katsuno M. Current perspectives on the diagnosis, assessment, and management of vasculitic neuropathy. Expert Rev Neurother. 2022;22(11-12):941-952. doi: 10.1080/14737175.2022.2166831
[16] Rodrigues CEM, Carvalho JF, Shoenfeld Y. Neurological manifestations of antiphospholipid syndrome. Eur J Clin Invest 2010;40:350-9. doi: 10.1111/J.1365-2362.2010.02263.X.
[17] Ricarte IF, Dutra LA, Abrantes FF, Toso FF, Barsottini OGP, Silva GS, et al. Neurologic manifestations of antiphospholipid syndrome. Lupus 2018;27:1404-14. doi: 10.1177/0961203318776110.
[18] Chiloiro S, Giampietro A, Bianchi A, De Marinis L. Empty sella syndrome: Multiple endocrine disorders. Handb Clin Neurol 2021;181:29-40. https://doi.org/10.1016/B978-0-12-820683-6.00003-8.
[19] Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P. Pituitary Apoplexy. Endocr Rev 2015;36:622-45. https://doi.org/10.1210/ER.2015-1042.
[20] Rajasekaran S, Vanderpump M, Baldeweg S, Drake W, Reddy N, Lanyon M, et al. UK guidelines for the management of pituitary apoplexy. Clin Endocrinol (Oxf) 2011;74:9-20. https://doi.org/10.1111/J.1365-2265.2010.03913.X.
[21] Makaryus AN, McFarlane SI. Diabetes insipidus: diagnosis and treatment of a complex disease. Cleve Clin J Med 2006;73:65-71. https://doi.org/10.3949/CCJM.73.l65.
[22] Ishii M. Neurologic complications of nondiabetic endocrine disorders. Continuum (Minneap Minn) 2014;20:560-79. https://doi.org/10.1212/01.CON.0000450966.68828.45.
[23] Tritos NA, Biller BMK. Cushing's disease. Handb Clin Neurol 2014;124:221-34. https://doi.org/10.1016/B978-0-444-59602-4.00015-0.
[24] Farrugia FA, Martikos G, Tzanetis P, Charalampopoulos A, Misiakos E, Zavras N, et al. Pheochromocytoma, diagnosis and treatment: Review of the literature. Endocr Regul 2017;51:168-81. https://doi.org/10.1515/ENR-2017-0018.
[25] Rodríguez I, Fluiters E, Pérez-Méndez LF, Luna R, Páramo C, García-Mayor R V. Factors associated with mortality of patients with myxoedema coma: prospective study in 11 cases treated in a single institution. J Endocrinol 2004;180:347-50. https://doi.org/10.1677/JOE.0.1800347.
[26] Dubbs SB, Spangler R. Hypothyroidism: causes, killers, and life-saving treatments. Emerg Med Clin North Am 2014;32:303-17. https://doi.org/10.1016/J.EMC.2013.12.003.
[27] Klubo-Gwiezdzinska J, Wartofsky L. Thyroid emergencies. Med Clin North Am 2012;96:385-403. https://doi.org/10.1016/J.MCNA.2012.01.015.
[28] Subekti I, Soewondo P, Soebardi S, Darmowidjojo B, Harbuwono DS, Purnamasari D, et al. Practical Guidelines Management of Graves Ophthalmopathy. Acta Med Indones 2019;51:364-71.
[29] Lee TG, Ha CK, Lim BH. Thyroid storm presenting as status epilepticus and stroke. Postgrad Med J 1997;73:61. https://doi.org/10.1136/PGMJ.73.855.61.
[30] Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: An update of its etiology, pathogenesis and management. Metabolism 2016;65:507-21. https://doi.org/10.1016/J.METABOL.2015.12.007.
[31] Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic Crises in Adult Patients With Diabetes. Diabetes Care 2009;32:1335. https://doi.org/10.2337/DC09-9032.
[32] Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, Bril V, Russell JW, Viswanathan V. Diabetic neuropathy. Nat Rev Dis Primers. 2019 Jun 13;5(1):41. doi: 10.1038/s41572-019-0092-1.
[33] Yong AW, Morris Z, Shuler K, Smith C, Wardlaw J. Acute symptomatic hypoglycaemia mimicking isch-aemic stroke on imaging: a systemic review. BMC Neurol 2012;12. https://doi.org/10.1186/1471-2377-12-139
[34] Heinz UE, Rollnik JD. Outcome and prognosis of hypoxic brain damage patients undergoing neurological early rehabilitation. BMC Res Notes 2015;8:243. https://doi.org/10.1186/S13104-015-1175-Z.
[35] Scala R. Hypercapnic encephalopathy syndrome: A new frontier for non-invasive ventilation? Respir Med 2011;105:1109-17. https://doi.org/10.1016/j.rmed.2011.02.004.
[36] Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 2005;171:340-7. https://doi.org/10.1164/RCCM.200406-763OC.
[37] Hoen B, Duval X. Clinical practice. Infective endocarditis. N Engl J Med 2013;368:1425-33. https://doi.org/10.1056/NEJMCP1206782/SUPPL_FILE/NEJMCP1206782_DISCLOSURES.PDF
[38] Ferro JM, Fonseca AC. Infective endocarditis. Handb Clin Neurol 2014;119:75-91. https://doi.org/10.1016/B978-0-7020-4086-3.00007-2.
[39] Jensen CW, Chen EP. Management of brain malperfusion in acute type A aortic dissection. Asian Cardiovasc Thorac Ann 2022;30:364-70. https://doi.org/10.1177/02184923211054693.
[40] Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE, et al. 2010 ACCF/AHA/AATS/ ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Soc. Circulation 2010;121. https://doi.org/10.1161/CIR.0B013E3181D4739E.
[41] Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, et al. Hepatic Encephalopathy in Chronic Liver Disease: 2014 Practice Guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J Hepatol 2014;61:642-59. https://doi.org/10.1016/J.JHEP.2014.05.042.
[42] Sureka B, Bansal K, Patidar Y, Rajesh S, Mukund A, Arora A. Neurologic Manifestations of Chronic Liver Disease and Liver Cirrhosis. Curr Probl Diagn Radiol 2015;44:449-61. https://doi.org/10.1067/J.CPRADIOL.2015.03.004.
[43] Hadjivassiliou M, Sanders DS, Grünewald RA, Woodroofe N, Boscolo S, Aeschlimann D. Gluten sensitivity: from gut to brain. Lancet Neurol 2010;9:318-30. https://doi.org/10.1016/S1474-4422(09)70290-X.
[44] Işikay S, Kocamaz H. The neurological face of celiac disease. Arq Gastroenterol 2015;52:167-70.https://doi.org/10.1590/S0004-28032015000300002.
[45] Balestrieri P, Ribolsi M, Guarino MPL, Emerenziani S, Altomare A, Cicala M. Nutritional Aspects in Inflammatory Bowel Diseases. Nutrients 2020;12. https://doi.org/10.3390/NU12020372.
[46] Ibitoye RT, Wilkins A, Scolding NJ. Neurosarcoidosis: a clinical approach to diagnosis and management. J Neurol 2017;264:1023-8. https://doi.org/10.1007/S00415-016-8336-4.
[47] Kaku M, Berk JL. Neuropathy Associated with Systemic Amyloidosis. Semin Neurol 2019;39:578-88. https://doi.org/10.1055/S-0039-1688994.
[48] Perfetto F, Casagrande S, Barilaro A, Di Gioia M, Santi R, Allinovi M, et al. Progressive and atypical neurological symptoms in refractory systemic AL amyloidosis. Intern Emerg Med 2021;16:1927-33. https://doi.org/10.1007/S11739-020-02489-8.
[49] Saitakis G, Chwalisz BK. The neurology of IGG4-related disease. J Neurol Sci 2021;424. https://doi.org/10.1016/J.JNS.2021.117420.
[50] Mauermann M.Neurologic Complications of Lymphoma, Leukemia, and Paraproteinemias. Continuum 2017;23:669-690. http://doi.org/10.1212/CON.0000000000000468